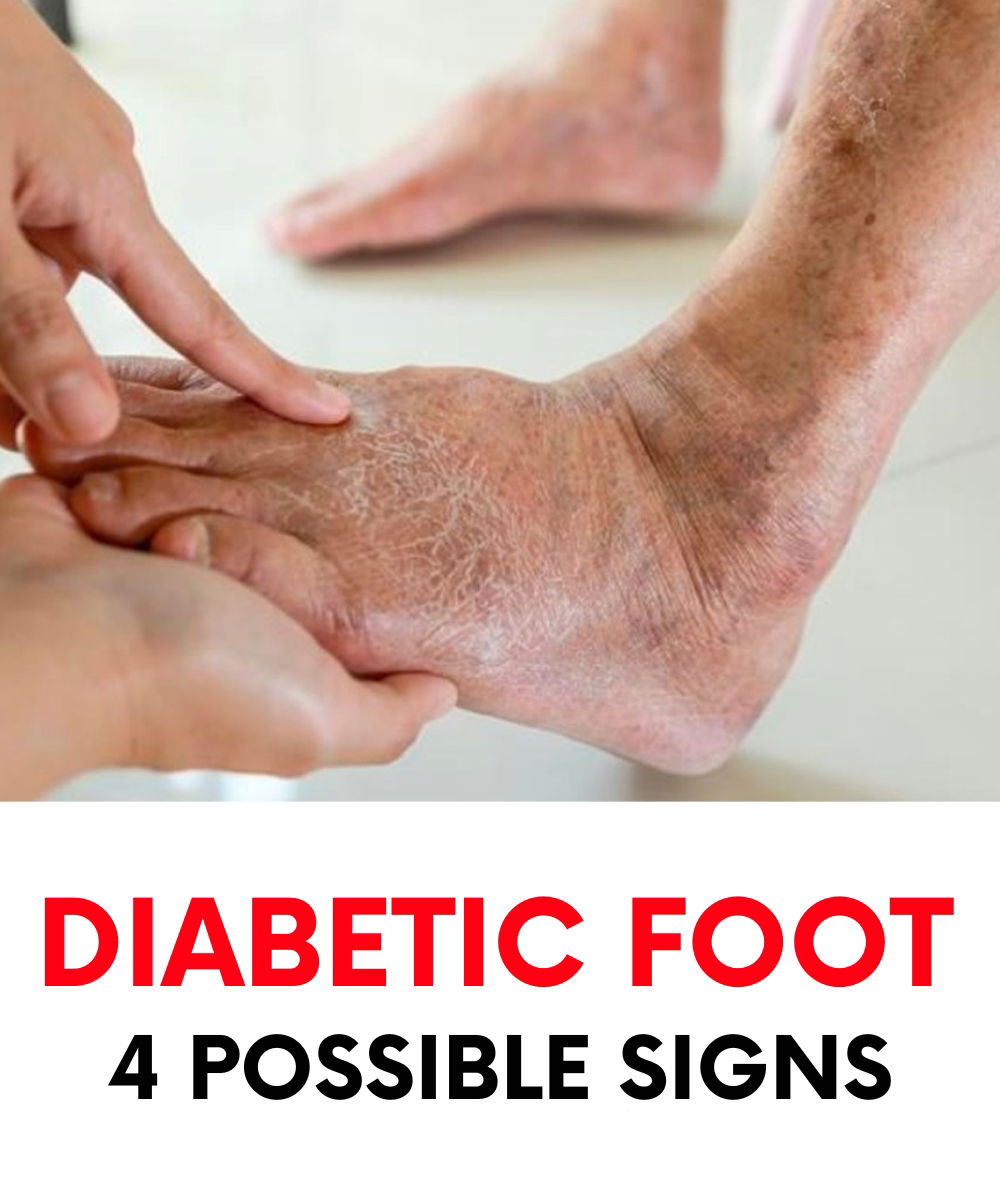
Diabetic foot is a potentially severe consequence of diabetes mellitus that often appears in the form of ulcers or sores on the feet, particularly ones that heal very slowly or not at all.
If you live with diabetes, it’s essential to regularly inspect your feet, between your toes, and along the soles.
Those who have had diabetes for many years, particularly type 1 diabetes, should pay extra attention to their lower limbs.
Feet are far from the heart and often the first to suffer from poor circulation, a common result of long-term diabetes. The condition affects blood flow, reducing the amount of oxygen reaching tissues in the lower body.
Over time, this lack of oxygen and nourishment can cause tissue damage and even necrosis—the death of body tissue.

What Is Diabetic Foot?
“Diabetic foot” describes a disabling condition involving structural and functional changes in the foot and ankle.
It usually stems from two main problems: nerve damage (neuropathy) and reduced blood flow due to artery blockages (ischemia).
Based on the underlying cause, diabetic foot is classified into two types:
- Neuropathic diabetic foot: This form is the result of nerve damage due to consistently high blood sugar levels. It affects sensory, motor, and autonomic nerves, leading to decreased sensation and altered foot structure. Without proper feeling in the feet, individuals are more likely to develop ulcers, especially on pressure points like the soles.

- Neuroischemic diabetic foot: This condition results from poor circulation due to narrowed or blocked arteries. It significantly reduces blood supply to the foot, making tissues more vulnerable to injury, infection, and gangrene.
Why Does Diabetic Foot Develop?
CONTINUE READING ON THE NEXT PAGE 🥰💕

